What is a cruciate Ligament
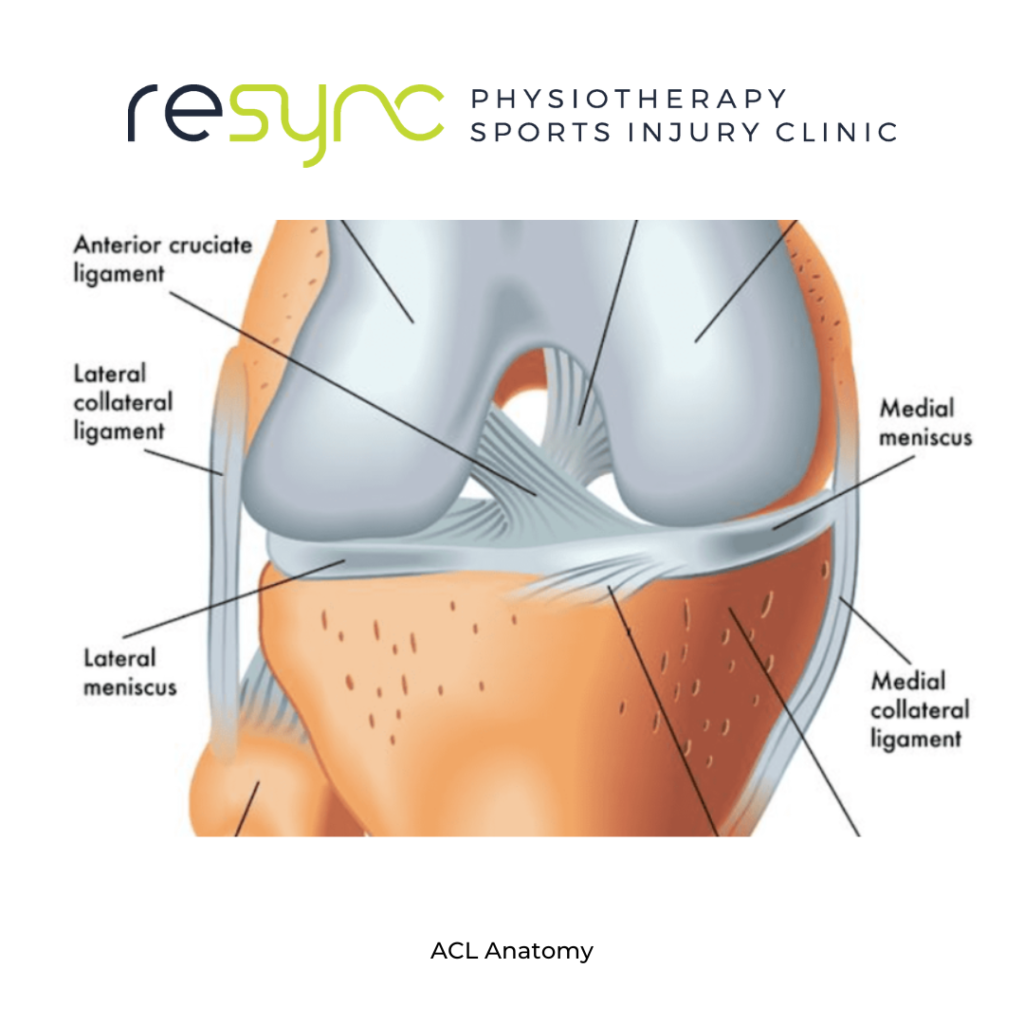
The cruciate ligaments are two ligaments in the knee that cross over each other and form an “X” shape. They are called the anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL).
The ACL is located in the front of the knee and helps to prevent the shin bone (tibia) from moving too far forward in relation to the thigh bone (femur). It also helps to stabilize the knee during quick changes in direction or landing from a jump.
The PCL is located in the back of the knee and helps to prevent the shin bone from moving too far backward in relation to the thigh bone. It also helps to control the rotation of the knee.
Both the ACL and PCL work together to provide stability to the knee and to prevent excessive movement between the thigh and shin bones. Injuries to these ligaments can occur as a result of a traumatic event such as a sports-related injury or a car accident. Symptoms of a cruciate ligament injury can include pain, swelling, stiffness, and instability in the knee. Treatment may include rest, ice, physical therapy, and in some cases, surgery.
How does a cruciate ligament get injured?
Cruciate ligaments, specifically the Anterior Cruciate Ligament (ACL) and the Posterior Cruciate Ligament (PCL) can be injured in a variety of ways, but some common causes include:
- Trauma: A direct blow to the knee, such as from a collision in contact sports or a car accident, can cause a cruciate ligament injury.
- Non-Contact injuries: These types of injuries can occur during sports or other physical activities that require sudden changes in direction, jumping or landing from a jump, or sudden stops and starts. These types of injuries are more common in sports like soccer, football, basketball, or skiing.
- Overuse: Repetitive stress on the knee joint can lead to small tears in the cruciate ligaments, which can eventually lead to a full tear if not treated properly.
- Degenerative conditions: As people age, the ligaments can become weaker and more susceptible to injury.
In general, a cruciate ligament injury can happen when the knee is forced to move in an unnatural direction and are most commonly caused by a rotational force. The ACL is more commonly injured than the PCL, but both can be damaged in the same type of trauma.
Symptoms of a cruciate ligament injury include pain, swelling, stiffness, and instability in the knee. If you suspect you have injured your cruciate ligament, it’s important to seek medical attention as soon as possible to receive a proper diagnosis and treatment plan.
ACL Rehab
ACL (anterior cruciate ligament) rehabilitation is a process of rebuilding the strength, flexibility, and stability of the knee following injury to the ACL. The ACL is one of the four major ligaments in the knee that provide stability to the joint. It can be injured through a variety of mechanisms, including sports-related activities, falls, or car accidents.
The goal of ACL rehabilitation is to restore the normal range of motion and strength of the knee, reduce pain and inflammation, and prevent re-injury. The rehabilitation process typically begins with a period of rest, ice, and anti-inflammatory medication to reduce pain and swelling.
Physical therapy is an important part of the ACL rehabilitation process, which may involve exercises to improve flexibility, strength, and balance. The exercises typically focus on the quadriceps, hamstrings, and calf muscles. Knee bracing may also be used to support the joint during the rehabilitation process.
The length of the rehabilitation process can vary depending on the severity of the injury and the individual’s response to treatment. It can take several months for the knee to fully heal and for the person to be able to return to normal activities.
It’s important to follow the instruction of physiotherapist and doctor closely to have a successful recovery.
What happens in an ACL Surgery?
ACL (anterior cruciate ligament) surgery is a procedure used to repair or reconstruct a torn or damaged ACL. The ACL is one of the four major ligaments in the knee that provide stability to the joint. A torn ACL can cause the knee to feel unstable, particularly when performing activities such as turning, cutting, or jumping.
There are two main types of ACL surgery: reconstruction and replacement.
ACL reconstruction is the most common type of surgery. In this procedure, the surgeon will remove the torn ACL and replace it with a tissue graft. The graft is typically taken from the patient’s own body, such as the patellar tendon (bone-tendon-bone) or the hamstring tendon. The graft is then secured to the bone with screws or other fixation devices.
ACL replacement is a newer option, where a synthetic graft are used to replace the torn ACL and fixated in the bone.
The surgery is typically performed using arthroscopy, which is a minimally invasive technique that uses small incisions and a camera to visualize the inside of the joint. The procedure typically takes around one to two hours and is performed under general anesthesia.
After the surgery, the patient will typically need to go through a period of rehabilitation to regain strength and range of motion in the knee. This can include physical therapy and exercises, as well as the use of crutches or a knee brace to support the joint.
Recovery can take several months, and the patient will need to follow the post-surgery guidelines given by the doctor and physiotherapist to avoid any further damage or complications.
What are the complications of ACL Surgery?
ACL (anterior cruciate ligament) surgery is generally considered a safe and effective procedure, but like any surgery, there are potential risks and complications that can occur. Some of the most common complications associated with ACL surgery include:
- Infection: Any surgical procedure carries a small risk of infection. This can be reduced by proper wound care and taking antibiotics as prescribed by the surgeon.
- Blood clots: Blood clots can form in the legs after surgery, which can be dangerous if they travel to the lungs. Patients may be given blood thinners to prevent this.
- Nerve or vessel damage: The surgical incisions are made close to nerves and vessels, and while very rare, it’s possible to cause damage to them during the surgery.
- Graft failure: The graft used to replace the torn ACL may not heal properly or may be re-injured.
- Stiffness: After the surgery, the knee may become stiff and have a reduced range of motion. Physical therapy can help to regain the motion
- Persistent pain: Some patients may continue to experience pain in the knee even after the surgery.
- Implant failure: There is a risk of failure for the artificial graft that is used in some cases.
It is important to be aware of these risks and to discuss them with your surgeon. Your surgeon will be able to explain the risks and benefits of the surgery, as well as what you can expect during the recovery process.
It’s important to follow the instructions of the surgeon, physiotherapist and doctor closely to have a successful recovery and to minimize the risk of complications.

ACL Rehab Protocol
An ACL (anterior cruciate ligament) rehabilitation protocol is a specific plan or set of guidelines that outlines the steps and exercises that should be followed in order to properly rehabilitate a knee following an ACL injury.
The protocol is usually tailored to the individual’s injury and recovery and can vary depending on the type of surgery (reconstruction or replacement) and the specific needs of the patient. However, in general, an ACL rehabilitation protocol usually includes the following phases:
- Preoperative phase: This phase begins before the surgery and may include exercises to improve the range of motion, muscle strength, and flexibility of the knee.
- Early postoperative phase: This phase starts immediately after the surgery and is focused on reducing pain and swelling, and regaining range of motion. Exercises in this phase include range of motion exercises, such as knee flexion and extension, as well as exercises to improve quadriceps activation.
- Intermediate postoperative phase: This phase is typically started 4-6 weeks after the surgery and focuses on building strength and stability in the knee. Exercises in this phase include progressive resistance exercises for the quadriceps, hamstrings, and calf muscles, as well as balance and proprioception exercises.
- Late postoperative phase: This phase is typically started 8-12 weeks after the surgery and focuses on returning to sport-specific activities. Exercises in this phase include sport-specific drills, agility training, plyometrics, and strength training.
- Return to sport phase: This phase is tailored to the individual athlete’s needs and goals, with the goal of returning to full sport participation. This includes sport-specific training, as well as testing to ensure that the knee has fully healed and that the athlete is able to perform at the same level as before the injury.
It’s important to remember that, the rehabilitation process is tailored to the individual’s injury, surgery type and recovery rate. Additionally, it’s important to work closely with a physiotherapist and/or a physician throughout the rehabilitation process. They will be able to guide you through each phase and help you progress through the protocol at the appropriate pace.
Guide to return to running after ACl Surgery
Returning to running after ACL (anterior cruciate ligament) surgery can be a long and challenging process. The timing and progression of the return to running should be determined by the individual’s injury, surgery type, and recovery rate, it’s important to work closely with a physiotherapist and/or doctor throughout the process.
Generally, the return to running is broken down into several phases. The specific details may vary depending on the individual, but an example guide is:
- Preoperative phase: The focus is on maintaining cardiovascular fitness and muscle strength in the legs. This may include activities such as cycling, swimming, and upper body strength training.
- Early postoperative phase: The focus is on controlling pain and swelling, regaining range of motion and quadriceps control. This may include exercises such as range of motion exercises, straight leg raises, and heel slides.
- Intermediate postoperative phase: The focus is on building strength and stability in the knee. This may include exercises such as leg press, leg extension, leg curl and single leg squat.
- Late postoperative phase: The focus is on sport-specific training, such as agility and plyometric exercises, as well as sport-specific drills.
- Return to Running phase: In this phase, you will gradually increase the distance and intensity of your running. Start with light jogging, then progress to running at a moderate pace, then running with change of direction and finally running with sudden stop and start.
It is important to progress gradually and not to rush the process, as this can lead to re-injury or complications. It’s essential to have regular check-ins with physiotherapist and/or doctor to monitor progress and make adjustments to the rehabilitation plan as needed.
It’s also worth noting that, return to running may take several months and some people may need additional time for complete recovery.
This Article was written by
Diarmuid Hegarty Clinical Specialist MSK Physio
MISCP, MSc Physio MSc Sports Med, EXOS S&C Specialist



