What is Shin Splints
Shin splints, medically known as medial tibial stress syndrome (MTSS), is a common condition characterized by pain and tenderness along the inside of the shinbone (tibia).
It frequently affects runners and athletes involved in activities that require repetitive impact on the lower legs. This article aims to provide relevant information on shin splints, including its causes, exercises that can help alleviate symptoms, and how physiotherapy plays a crucial role in reducing the recurrence of shin splints.
Here is the science bit about Shin Splints or medial tibial stress syndrome (MTSS). When searching for a cause of shin splints it is important to consider the complex interplay of factors involved in its development. While the exact mechanism is not fully understood, several contributing factors have been identified:
- Repetitive Microtrauma: The primary cause of MTSS is repetitive microtrauma to the tissues surrounding the tibia, including the muscles, tendons, and periosteum (outer layer of bone). Activities that involve repetitive impact or excessive stress on the lower leg, such as running, jumping, or dancing, can lead to the accumulation of microtrauma over time.
- Overloading and Overuse: MTSS often occurs due to overloading and overuse of the lower leg muscles. When the intensity, duration, or frequency of physical activity exceeds the body’s ability to adapt and recover, the muscles and associated structures become fatigued. This fatigue leads to altered biomechanics and an increased risk of tissue damage.
- Biomechanical Factors: Individuals with certain biomechanical characteristics may be more susceptible to developing MTSS. Factors such as overpronation (excessive inward rolling of the foot), flat feet, high arches, leg length discrepancies, or poor running technique can result in abnormal distribution of forces along the lower leg, leading to increased stress on the tibia.
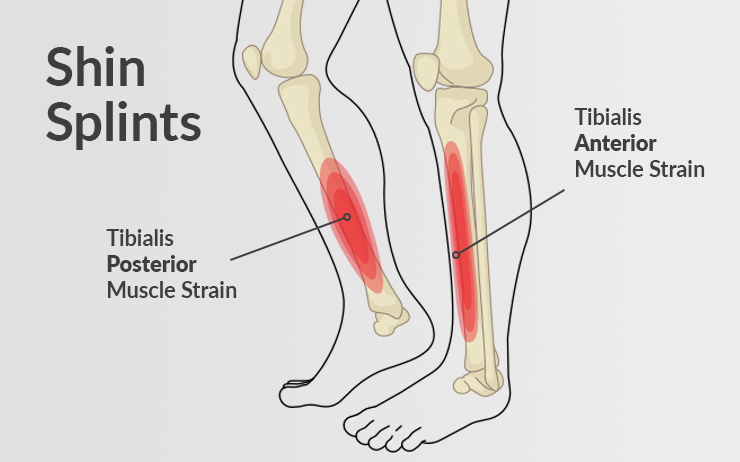
- Muscle Imbalances: Imbalances between the anterior and posterior leg muscles, particularly the tibialis anterior (front of the leg) and the calf muscles (gastrocnemius and soleus), can contribute to the development of MTSS. Weakness or tightness in these muscles can alter the mechanics of the lower leg and increase the strain on the tibial tissues.
- Decreased Shock Absorption: Insufficient shock absorption capacity of the lower leg may also play a role in MTSS. If the muscles and soft tissues are unable to adequately absorb the impact forces generated during weight-bearing activities, the tibia may experience increased stress, leading to inflammation and pain.
The repetitive microtrauma and excessive stress on the tibia lead to an inflammatory response within the affected tissues. This inflammation can cause pain, swelling, and tenderness along the inner edge of the shin. With continued stress and inadequate recovery, the body’s natural healing mechanisms may become overwhelmed, resulting in the development of MTSS.
It is important to note that the pathophysiology of MTSS is multifactorial, and individual variations in biomechanics, training methods, and other factors contribute to its development. Understanding these underlying factors can help guide treatment approaches, including exercise interventions and physiotherapy, to address the root causes and promote healing and prevention of MTSS.
Shin Splints in Runners
Shin splints, a common condition among runners, refers to the pain and discomfort experienced along the inner edge of the shinbone (tibia). It is often associated with repetitive stress and overuse of the lower leg during running or other high-impact activities. Here are some key points about shin splints in runners:
Causes Of Shin Splints in Runners
Overuse and Increased Intensity: Sudden or excessive increases in training volume, intensity, or frequency can overload the muscles, tendons, and bone tissue in the lower leg, leading to shin splints. High Impact sports and endurance athletes are also susceptible to shin splints.
Biomechanical Factors: Runners with flat feet, high arches, or abnormal foot pronation (overpronation or supination) may be more susceptible to shin splints due to altered forces along the lower leg. The strongest muscle in the lower shin area is the Soleus Muscle. The muscles have connective tissues which then attaches to medial portion of the tibia.
Improper Footwear: Wearing worn-out shoes or shoes that lack proper support and cushioning can contribute to the development of shin splints. Shock absorbing insoles are recommended to help reduce stress adn ease pain in the shin bone.
Running Surface: Repeatedly running on hard or uneven surfaces, such as concrete or asphalt, increases the impact on the lower leg and may contribute to shin splints as harder surfaces are more aggressive on the muscles and shin bone during running.
Gradual Progression: Gradually increasing training volume, intensity, and distance allows the muscles, tendons, and bones to adapt to the demands of running, reducing the risk of shin splints.
Proper Footwear: Choosing running shoes that provide adequate support, cushioning, and shock absorption based on individual foot type and gait can help prevent shin splints.
Running Surface: Varying running surfaces and incorporating softer terrain (e.g., grass, trails) can help reduce the repetitive impact on the lower leg. d. Strength and Conditioning: Incorporating strength training exercises, particularly for the lower leg muscles (e.g., calf raises, toe curls), can improve muscle strength and stability, reducing the strain on the shinbone.

Shin Splints and Stress Fractures
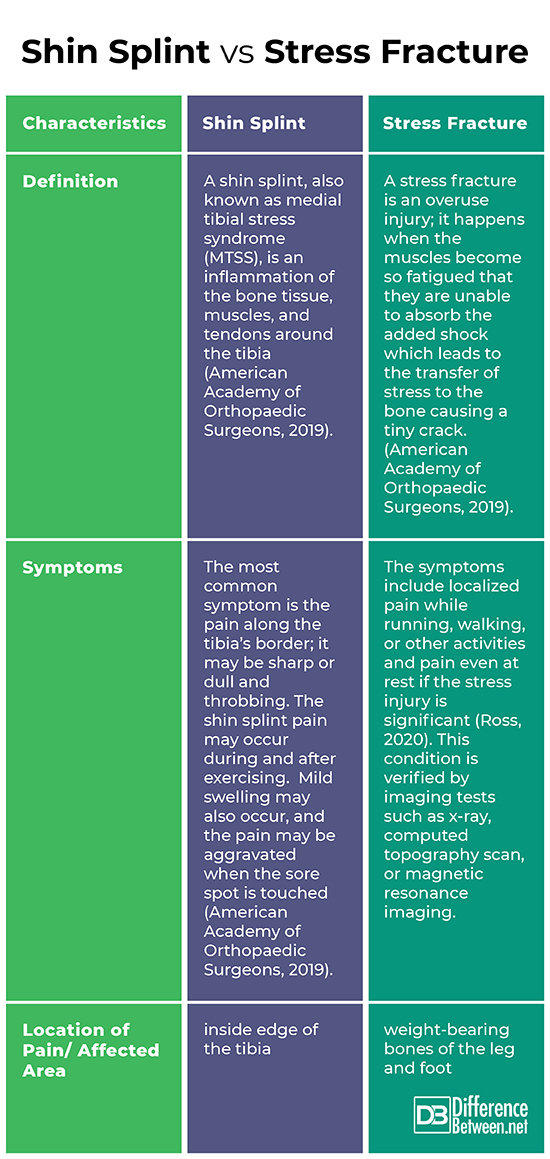
Shin splints and stress fractures are two distinct but related conditions that can affect the lower leg. While shin splints involve inflammation and irritation of the soft tissues around the shinbone, stress fractures refer to small cracks or breaks in the bone itself. Shin splints can potentially lead to stress fractures if not properly managed. Here’s how it can happen:
Overuse and Continued Stress: Shin splints often occur due to repetitive stress and overuse of the lower leg, especially during activities like running or jumping. If the underlying cause of shin splints, such as training errors or biomechanical issues, is not addressed, the excessive stress on the lower leg can persist.
Altered Biomechanics: Shin splints can be associated with biomechanical abnormalities like overpronation (excessive inward rolling of the foot) or high-impact forces on the leg. These factors can lead to increased strain on the tibia, making it more susceptible to stress fractures over time.
Weakening of Bone Tissue: Prolonged or severe shin splints can lead to chronic inflammation and repetitive microtrauma to the bone, weakening the bone tissue in the affected area. The continuous stress and inadequate recovery can impair the bone’s ability to remodel and repair itself, making it more vulnerable to developing stress fractures.
Progression of Symptoms: If shin splints are not properly managed or if the individual continues to engage in high-impact activities without sufficient rest and recovery, the pain and symptoms may worsen. The persistent pain, often localized along the shinbone, can be an indication of an underlying stress fracture rather than just shin splints.
Diagnosis and Treatment: It is crucial to differentiate between shin splints and stress fractures to ensure appropriate treatment. Stress fractures typically present with localized pain, tenderness, and swelling over a specific area of the bone. Imaging techniques like X-rays or bone scans may be necessary to confirm the diagnosis. Treatment for stress fractures usually involves immobilization, rest, and gradual return to activity under medical supervision.
To prevent shin splints from progressing to stress fractures, it is essential to address the underlying causes of shin splints, such as training errors, improper footwear, and biomechanical issues. This may involve modifying training routines, wearing supportive shoes, incorporating strength and flexibility exercises, and seeking professional guidance from a healthcare provider or a sports medicine specialist. It’s important to listen to your body, give it adequate rest and recovery, and seek medical attention if symptoms persist or worsen.
Exercises for Shin Splints:
- Rest and Ice/ cold packs: Initially, it is important to allow adequate rest for the affected leg to reduce pain and inflammation. Applying ice packs for 15-20 minutes at regular intervals can further alleviate swelling.
- Stretching: Gentle stretching exercises targeting the calf muscles, Achilles tendon, and the front of the lower leg can help improve flexibility and relieve tension on the shinbone. Examples include toe raises, calf stretches, and ankle dorsiflexion exercises.
- Strengthening Exercises: Strengthening the muscles in the lower leg and foot can help reduce the strain on the shinbone. Toe curls, heel walking, and resistance band exercises for the foot and ankle are beneficial for improving muscle strength and stability.
- Cross-Training: Engaging in low-impact activities like swimming, cycling, or using an elliptical machine can maintain cardiovascular fitness while reducing the stress on the shins. It allows for active recovery while avoiding excessive impact.

Shin Splints Treatment
Physiotherapy plays a vital role in the management and prevention of shin splints. A physiotherapist can provide an individualized treatment plan tailored to specific needs. Here are some common interventions used in physiotherapy:
- Biomechanical Assessment: A thorough examination of your running or walking gait, foot arch, and leg alignment can help identify any underlying issues contributing to shin splints. Custom orthotics or shoe recommendations may be provided to improve biomechanics and reduce strain on the shins.
- Manual Therapy: Techniques like massage, myofascial release, and joint mobilization can help relieve muscle tightness, improve circulation, and reduce pain in the affected area.
- Exercise Prescription: A physiotherapist can design a comprehensive exercise program that includes stretching, strengthening, and proprioception exercises to address muscle imbalances, enhance flexibility, and improve overall lower limb stability.
- Gait Analysis and Running Technique: Analyzing running technique can identify any biomechanical flaws that contribute to shin splints. The physiotherapist can provide guidance on proper running form, stride length, foot strike, and cadence to reduce strain on the shins.
- Gradual Return to Activity: A physiotherapist can guide you through a structured rehabilitation plan, gradually increasing activity levels to prevent re-injury and ensure a safe return to running or sports.
Conclusion: Shin splints can be a painful setback for runners and athletes, but with the right approach, it is manageable and preventable. By incorporating exercises targeting flexibility, strength, and stability, along with seeking guidance from a physiotherapist, individuals can reduce symptoms, enhance recovery, and minimize the likelihood of shin splints recurring. Remember to consult a healthcare professional for an accurate
This Article was written by Diarmuid Hegarty our Clinical Specialist MSK Physiotherapy
If you wish to book an appointment with Diarmuid you can do so via this link or call the clinic on 01-6855181

